[cs_content][cs_element_section _id=”1″ ][cs_element_layout_row _id=”2″ ][cs_element_layout_column _id=”3″ ][cs_text]
News and stories from IFCHC member Community Health Centres and CHC associations around the world. In this issue, a focus on COVID-19 responses from our members globally. Scroll down to bottom of newsletter for list of current IFCHC members.
Click here for information on becoming a member
[/cs_text][/cs_element_layout_column][cs_element_layout_column _id=”5″ ][x_image type=”none” src=”https://www.ifchc.org/wp-content/uploads/2020/08/NHCW20-FB-header.png” alt=”” link=”true” href=”https://healthcenterweek.org/” title=”” target=”blank” info=”popover” info_place=”top” info_trigger=”hover” info_content=”U.S. National Community Health Center Week (August 9-15)”][cs_text]
Happy National Community Health Centers Week to our U.S. Members!
[/cs_text][/cs_element_layout_column][/cs_element_layout_row][cs_element_layout_row _id=”8″ ][cs_element_layout_column _id=”9″ ][cs_element_line _id=”10″ ][/cs_element_layout_column][/cs_element_layout_row][/cs_element_section][cs_element_section _id=”11″ ][cs_element_layout_row _id=”12″ ][cs_element_layout_column _id=”13″ ] [/cs_element_layout_column][cs_element_layout_column _id=”14″ ][cs_text]
Battling the COVID-19 Pandemic on the Frontlines in South Los Angeles, USA
[/cs_text][/cs_element_layout_column][cs_element_layout_column _id=”16″ ] [/cs_element_layout_column][/cs_element_layout_row][cs_element_layout_row _id=”17″ ][cs_element_layout_column _id=”18″ ][x_columnize]
 Located in south Los Angeles (South LA), California, USA, St. John’s Well Child & Family Center is a network of 19 federally-qualified Community Health Centres providing care and support to a wide range of community members within the largest area of poverty in the United States.
Located in south Los Angeles (South LA), California, USA, St. John’s Well Child & Family Center is a network of 19 federally-qualified Community Health Centres providing care and support to a wide range of community members within the largest area of poverty in the United States.
This multi-faceted Community Health Centre has been steadfastly committed to responding to the desperate need for COVID-19 services locally. Decades of racial and social inequality have resulted in a disproportionately high incidence of COVID-19 among South LA’s predominantly Latinx and African-American population. In fact, 47% of COVID-19 deaths come from the Latinx community in Los Angeles County while African-Americans represent 11% of all COVID-19 deaths but only 8% of the population.
To reduce the pandemic’s impact, St. John’s responded swiftly and decisively in early March when the first cases of community transmission were reported. South Los Angeles is home to more than 1.5 million people and has the highest poverty rates in the United States.
“To successfully control COVID-19, we mobilized early to keep all of our communities safe and healthy,” affirms Jim Mangia, President and Chief Executive Officer of St. John’s. “We needed to marshal our resources to help the most vulnerable first to reduce infection rates and keep our community safe.”
 St. John’s started by addressing the safety of its 600 staff and over 85,000 patients at 17 fixed sites and two mobile clinics. An internal COVID-19 Preparation Task Force was convened, comprised of key staff from every department, who led the complete retooling of the organization and redesigned every system and workflow in response to the pandemic.
St. John’s started by addressing the safety of its 600 staff and over 85,000 patients at 17 fixed sites and two mobile clinics. An internal COVID-19 Preparation Task Force was convened, comprised of key staff from every department, who led the complete retooling of the organization and redesigned every system and workflow in response to the pandemic.
St. John’s purchased Personal Protective Equipment (PPE) from national and international sources and received in-kind donations as well, enabling the agency to secure a six-month stockpile of PPE and sanitation supplies. Facilities staff erected isolation tents outside each fixed site to conduct testing and triage. Patients were screened and provided with face masks and screened before entering the clinics.
St. John’s initially had extremely limited access to COVID-19 testing kits at the beginning of the pandemic, especially in comparison with more affluent areas of the city. With support from local and state government agencies, augmented by St. John’s persistence in finding a new partner for test kits, the organization was able to secure enough kits to offer COVID-19 tests to everyone.
St. John’s started testing in late March. By early April, they were testing 600 residents of south Los Angeles each day. To date, St. John’s has tested 30,000 people for COVID-19 with a positivity rate of 16.63%. St. John’s is now one the largest providers of COVID testing and services of any Community Health Centre in the county.
 Patients who test positive are scheduled for follow-up medical appointments (either telehealth or face-to-face depending on patient needs). In addition, St. John’s established a telehealth Command Center, comprised of five teams of receptionists, medical assistants, and providers. Command Center staff respond to all COVID-related calls from patients and community members, answering questions, assessing any symptoms, and scheduling them as needed for testing and/or a full consultation.
Patients who test positive are scheduled for follow-up medical appointments (either telehealth or face-to-face depending on patient needs). In addition, St. John’s established a telehealth Command Center, comprised of five teams of receptionists, medical assistants, and providers. Command Center staff respond to all COVID-related calls from patients and community members, answering questions, assessing any symptoms, and scheduling them as needed for testing and/or a full consultation.
A Contact Tracing initiative was implemented to support the massive testing campaign that St. John’s is conducting. Contact Tracers call every COVID-positive patient to interview them regarding the people with whom they have been in contact. They then call each of those contacts to inform them of their exposure, provide them with education, answer their questions and assess them for symptoms. The initiative started in May to slow down the virus spread and identify potential viral clusters. To date, the initiative has contacted 25,366 individuals and scheduled 16,760 of the contacts for COVID-19 tests.
St. John’s started offering telehealth medicine to patients in late March to allow for continued service provision, initially conducted through telephony, Zoom, WhatsApp and FaceTime. A grant from the U.S. Federal Communications Commission allowed for the implementation of telehealth services that interface with St. John’s Electronic Health Record system as well as provide remote monitoring of patients with positive COVID tests and symptoms. Telehealth allows continued access to quality care for a community with limited available resources while helping reduce COVID-19 infection rates.
“The financial cost to St. John’s for responding to this pandemic is high,” says Mr. Mangia. “But the cost of not responding will be unfathomable and devastating to our community and its future. With the support of our partners, we will continue to respond as long as needed to keep South LA safe.”
[/x_columnize][/cs_element_layout_column][/cs_element_layout_row][cs_element_layout_row _id=”20″ ][cs_element_layout_column _id=”21″ ] [/cs_element_layout_column][cs_element_layout_column _id=”22″ ][cs_text]
Community Health Mobilizes in Melbourne, Australia
[/cs_text][/cs_element_layout_column][cs_element_layout_column _id=”24″ ] [/cs_element_layout_column][/cs_element_layout_row][cs_element_layout_row _id=”25″ ][cs_element_layout_column _id=”26″ ][x_columnize]
 Star Health is a registered Community Health Centre located within the inner urban southeast of metropolitan Melbourne, Australia. In June 2020, the Victoria State Department of Health and Human Services (DHHS) asked Star Heath to run a COVID-19 community engagement and health promotion program in public housing across local municipalities, targeting public housing and other vulnerable communities.
Star Health is a registered Community Health Centre located within the inner urban southeast of metropolitan Melbourne, Australia. In June 2020, the Victoria State Department of Health and Human Services (DHHS) asked Star Heath to run a COVID-19 community engagement and health promotion program in public housing across local municipalities, targeting public housing and other vulnerable communities.
“It became clear that outreach testing along with community engagement and support was going to be required,” says Sarah Fair, Star Health’s General Manager for Healthy Communities. “We needed to integrate several components into a robust program”.
As a result, Star Health created a Mobile COVID Testing Team (MCTT). Within the first 3 weeks of operations the team implemented 5 pop-up clinics per week. The organisation was then asked by the Regional Director of DHHS to ‘supercharge’ operations. This saw the creation of 13 clinics, spread across various locations, including extending operations in larger public housing high-rise buildings.
The focus of its program has been modified to cover other vulnerable communities including community housing projects, indigenous people, injecting drug users, sex workers and novel locations (for example near homelessness food services). A Testing Bus has been created to accommodate the requirements of a roving testing team.
 The MCTT also provides free transport for community members to fixed testing clinics 7 days a week in partnership with St Johns Ambulance. In addition, Star Health provides a Stay Connected line which offers psychosocial support, primary care and care coordination to any vulnerable community member during the pandemic.
The MCTT also provides free transport for community members to fixed testing clinics 7 days a week in partnership with St Johns Ambulance. In addition, Star Health provides a Stay Connected line which offers psychosocial support, primary care and care coordination to any vulnerable community member during the pandemic.
Star Health, in partnership with DHHS Office of Housing, has also established a Health Concierge Service at entry/exit points at three of the largest public housing communities. This service provides: community engagement, education, screening, masks and voluntary temperature checks and referrals.
 Between June 25 and July 23, the Star Health Mobile COVID Testing Team had conducted 1286 tests across public housing communities using a nurse-led model. This has seen over 50% testing coverage at some sites with over 1600 community engagements. The impacts of this work include reassuring epidemiological data on low case numbers, prevention education and linkage to care and support for many residents at risk across domains such as chronic condition care, mental health and food security.
Between June 25 and July 23, the Star Health Mobile COVID Testing Team had conducted 1286 tests across public housing communities using a nurse-led model. This has seen over 50% testing coverage at some sites with over 1600 community engagements. The impacts of this work include reassuring epidemiological data on low case numbers, prevention education and linkage to care and support for many residents at risk across domains such as chronic condition care, mental health and food security.
In addition to mobile testing, as of July 23, Star Health’s fixed site COVID-19 Screening Clinic has tested over 10,000 members of the local community. “Community Health Services like ours, throughout Victoria, are very well positioned to help within these challenging times,” says Star Health’s Acting CEO, Kent Burgess.
“Our organizations have deep, local relationships, with the capacity to effectively engage with diverse segments of the community.”
As a result of these long-standing relationships in their communities, Community Health Centres like Star Health tend to have have high levels of trust and better engagement with the community, including educational programs.
Star Health has collaborated closely with social landlords (public housing managers) and used the expertise of Star Health’s Public Housing Community Capacity Building team to develop a door-to-door testing model that outreaches from the pop-up clinics. Star Health has engaged with interpreters to help support vulnerable communities who may otherwise miss out on testing. It has also produced health educational/testing promotion videos in multiple community languages to support vulnerable people who are culturally and linguistically diverse.
Community Health Centres, throughout Victoria State and more broadly in Australia, are proving their critical value to the public health system during a time when the health system is being severely tested. No one can connect communities to health care and support like community health can.
[/x_columnize][/cs_element_layout_column][/cs_element_layout_row][cs_element_layout_row _id=”28″ ][cs_element_layout_column _id=”29″ ] [/cs_element_layout_column][cs_element_layout_column _id=”30″ ][cs_text]
Community Health Leads Expanded COVID-19 Efforts in Soweto/Johannesburg, South Africa
[/cs_text][/cs_element_layout_column][cs_element_layout_column _id=”32″ ] [/cs_element_layout_column][/cs_element_layout_row][cs_element_layout_row _id=”33″ ][cs_element_layout_column _id=”34″ ][x_columnize]
 When South Africa’s National Party took power in 1948 and introduced apartheid they also eliminated an impressive network of more than 40 Community Health Centres that had been established through the leadership of Drs Sidney and Emily Kark. The most famous of these was the first Community Health Centre, established by the Karks in the rural Kwa-Zulu Natal province town of Pholela.
When South Africa’s National Party took power in 1948 and introduced apartheid they also eliminated an impressive network of more than 40 Community Health Centres that had been established through the leadership of Drs Sidney and Emily Kark. The most famous of these was the first Community Health Centre, established by the Karks in the rural Kwa-Zulu Natal province town of Pholela.
Decades later, the post-apartheid government of South Africa implemented District Health Services with so-called “CHCs” as a key component. However, these CHCs lack many critical functions of “community-oriented primary health care (COPHC)” that are common to the CHC model around world.
That’s why, in 2013, Chiawelo Community Practice (CCP) was established within the Chiawelo CHC in Soweto, Johannesburg as an effort to begin re-building the true CHC model including COPHC. In concert with the Chiawelo CHC, Chiawelo Community Practice serves a community of ±22,000 people and is staffed by a part-time family physician, a clinical associate, two intern doctors rotating weekly, and more than 20 Community Health Workers (CHWs) who work under the guidance of a junior nurse team leader.
The Chiawelo Community Practice team delivers people-centred care to ±1,000 patients per month, with CHWs playing a critical role in health promotion, community engagement, and continuity of care. This has included setting up five health clubs in the community with ±150 elderly chronic patients involved in daily exercise, diet, and social sessions to combat social isolation.
With the onset on COVID-19, CHWs have been relied on heavily to support clients and the community. As part of their daily outreach activities, linking community members with services at the Chiawelo Community Practice clinic, CHWs have integrated COVID-19 screening. Each CHW aims for a daily goal of 14 client screenings, in addition to their other daily activities. CHWs have also been critical in staffing COVID-19 screening stations at the entrance of Chiawelo CHC and other clinics throughout Soweto.
Given the elevated risks from COVID-19 to patients with chronic and immuno-compromised conditions, Johannesburg region health authorities have tapped the team at Chiawelo Community Practice to expand home-based care and delivery of medications.
“We have a lot of experience to draw from already,” says Dr, Shabir Moosa, lead physician responsible for creation of Chiawelo Community Practice. “We have taken lessons and practices developed here and have developed a home-based Case Management Plan for chronic care patients throughout Johannesburg.”
Led by nursing team leaders, with delivery of medicines by CHWs, the plan is slated for roll out this August, with scale-up across Johannesburg over the months ahead.
[/x_columnize][/cs_element_layout_column][/cs_element_layout_row][cs_element_layout_row _id=”36″ ][cs_element_layout_column _id=”37″ ] [/cs_element_layout_column][cs_element_layout_column _id=”38″ ][x_custom_headline level=”h4″ looks_like=”h3″ accent=”false” class=”cs-ta-center”]Victoria, Canada’s Cool Aid Turns on a Dime[/x_custom_headline][/cs_element_layout_column][/cs_element_layout_row][cs_element_layout_row _id=”40″ ][cs_element_layout_column _id=”41″ ][x_columnize]

Some members of Cool Aid’s medical and health team stand together, while apart, in Victoria, Canada during COVID-19.
When your Community Health Centre has 20 locations, a staff compliment of 350, and 12,000 clients to support who are marginalized, many experiencing homelessness, it’s hard to turn on a dime. But that’s exactly what Victoria Cool Aid Society (Victoria, British Columbia, Canada) did when public health authorities ordered a shut down of businesses and many services throughout the province of British Columbia during the onset of the COVID-19 pandemic.
Day by day, the organization’s Health & Safety Manager and medical staff created new procedures to protect staff and clients from COVID-19. Staff focused on information technology made it possible for team members to quickly transition to working from home, leaning heavily on video conferencing. Human resources team members helped dozens of staff work through challenges and fears.
Cool Aid provided telemedicine options for patients, working with the provincial government to rapidly expand their Health Outreach Team to care for and support homeless and street-involved clients, both at usual encampments and new indoor spaces created as a result of the pandemic. As a Community Health Centre with tremendous focus on shelter and housing, Cool Aid also took on a new project to house 30 homeless individuals who had been camping in the city, receiving approval to build an additional 102 affordable apartment units. Housing is health care.
Several branches of the CHC went virtual, including their Downtown Community Centre and Support Services. Staff reported that relationships with clients actually deepened in many instances as clients sought and received assurances and safety information.
Riley Vaskic, an Outreach Worker at Cool Aid, notes that while COVID-19 has, unfortunately, reduced some services for clients due to physical distancing and precautions she has also seen many positive developments.
“The pandemic has shed a lot of light for the general public on homelessness and fewer people are turning a blind eye on our clients,” Vaskic says. “They are starting to realize that the health of the most marginalized affects the health of everyone. People better understand the critical role that housing plays in health and community wellbeing.”
She also says she’s pleased that jobs that have not traditionally been recognized as frontline are now being valued more profoundly. Important jobs like the ones played by her team at Cool Aid’s REES Support Services. Team members at REES take a co-operative, recovery-based approach to help reduce people’s isolation, providing people a resource centre with accessible computers & phone, employment preparation and labour pool jobs, and assistance and advocacy navigating income assistance, disability claims, identification, and more.
“We have learned new ways of connecting with people at Cool Aid and the pandemic has illuminated what really matters in my life.”
[/x_columnize][/cs_element_layout_column][/cs_element_layout_row][/cs_element_section][cs_element_section _id=”43″ ][cs_element_layout_row _id=”44″ ][cs_element_layout_column _id=”45″ ] [/cs_element_layout_column][cs_element_layout_column _id=”46″ ][x_custom_headline level=”h2″ looks_like=”h3″ accent=”false” class=”cs-ta-center” style=”color: hsl(0, 0%, 100%);”]Video and blog series from Canadian Association of Community Health Centres addresses inequitable health and social impacts of pandemic[/x_custom_headline][/cs_element_layout_column][cs_element_layout_column _id=”48″ ] [/cs_element_layout_column][/cs_element_layout_row][cs_element_layout_row _id=”49″ ][cs_element_layout_column _id=”50″ ][cs_text]
Homelessness
[/cs_text][/cs_element_layout_column][cs_element_layout_column _id=”52″ ][cs_text]
Domestic Violence
[/cs_text][/cs_element_layout_column][cs_element_layout_column _id=”54″ ][cs_text]
Isolated Seniors
[/cs_text][/cs_element_layout_column][cs_element_layout_column _id=”56″ ][cs_text]
Food Insecurity
[/cs_text][/cs_element_layout_column][/cs_element_layout_row][cs_element_layout_row _id=”58″ ][cs_element_layout_column _id=”59″ ][x_video_embed no_container=”true” type=”16:9″][/x_video_embed][/cs_element_layout_column][cs_element_layout_column _id=”61″ ][x_video_embed no_container=”true” type=”16:9″][/x_video_embed][/cs_element_layout_column][cs_element_layout_column _id=”63″ ][x_video_embed no_container=”true” type=”16:9″][/x_video_embed][/cs_element_layout_column][cs_element_layout_column _id=”65″ ][x_video_embed no_container=”true” type=”16:9″][/x_video_embed][/cs_element_layout_column][/cs_element_layout_row][cs_element_layout_row _id=”67″ ][cs_element_layout_column _id=”68″ ][cs_text]BLOG: Community Health Centres take swift action to protect Canada’s homeless during the pandemic[/cs_text][/cs_element_layout_column][cs_element_layout_column _id=”70″ ][cs_text]BLOG: Community Health Centres address surge in domestic violence, call for attention to systemic impacts of COVID-19[/cs_text][/cs_element_layout_column][cs_element_layout_column _id=”72″ ][cs_text]BLOG: Community Health Centres provide critical lifeline for isolated seniors during the pandemic[/cs_text][/cs_element_layout_column][cs_element_layout_column _id=”74″ ][cs_text]BLOG: Community Health Centres tackle surge in food insecurity across Canada during pandemic[/cs_text][/cs_element_layout_column][/cs_element_layout_row][/cs_element_section][cs_element_section _id=”76″ ][cs_element_layout_row _id=”77″ ][cs_element_layout_column _id=”78″ ][cs_text]
Bromley by Bow Centre mobilizes social prescribing crisis response in London, UK
 The Bromley by Bow Centre was one of the earliest pioneers of social prescribing principles and the London, UK based Community Health Centre aims to apply them in everything they do. This includes managing crisis situations.
The Bromley by Bow Centre was one of the earliest pioneers of social prescribing principles and the London, UK based Community Health Centre aims to apply them in everything they do. This includes managing crisis situations.
For the CHC’s skilled social prescribing Link Workers this means taking time to get to know a person, giving them space to make sense of their situation and feelings, then jointly developing a plan to help the person access the right information and support.
Social prescribing was developed in recognition that the majority of factors affecting mental and physical ill health are social and economic. People need friends and a feeling of belonging, a sense of purpose, financial security, a safe home and hope for their future. The term refers to a process whereby healthcare professionals refer patients to a range of local, non-clinical services in order to improve their health and wellbeing.
Bromley by Bow’s social prescribing service is usually triggered by a referral from a health professional. However, during the COVID-19 crisis, a combined Health Partnership and Social Prescribing team at the centre began a project to actively reach out to patients. People were identified, using health data and local knowledge, as having additional risk of social and economic vulnerability due to lock down measures.
People were contacted by the social prescribing health team by phone. These phone calls were widely welcomed and uncovered a higher level of distress and need than was expected with many respondents living on their own and feeling isolated and scared. Many people required help for essential needs such as food deliveries and help with accessing health advice. They also needed reassurance during an anxious time and a sense they were not alone. The organization developed a “Home Pack” to support local community members with online resources.

Food bank set up at Bromley by Bow Centre, one of many important services scaled through social prescribing crisis response.
During a ten-week period from late March to early June, 704 calls were made and 512 people in the age range of 9- 90 years were spoken with by team members. These were people who may not otherwise have been contacted during lock down and many were suffering in silence.
Once the social prescribing health team engaged with people, they were able to activate emergency food supplies from the Food Bank and other services from the organization and partner agencies.
Many local residents report that it was the conversation itself, the human connection, that they valued most valued during a troubling time. An interim report from the centre details a wide range of observations, outcomes, and lessons learned from the COVID-19 social prescribing crisis response.
[/cs_text][/cs_element_layout_column][cs_element_layout_column _id=”80″ ][cs_text]
America’s CHCs lead national testing and care efforts for vulnerable communities
 Since COVID-19 struck, Community Health Centers in rural and urban areas across the U.S. have pivoted to address the pandemic, launching drive-through and curbside testing sites and delivering 160,000 COVID tests per week. According to the latest research and findings from the U.S. National Association of Community Health Centers, 94% of America’s more than 1,400 Community Health Centers have the ability to test and 79% are providing walk-up or drive-up testing.
Since COVID-19 struck, Community Health Centers in rural and urban areas across the U.S. have pivoted to address the pandemic, launching drive-through and curbside testing sites and delivering 160,000 COVID tests per week. According to the latest research and findings from the U.S. National Association of Community Health Centers, 94% of America’s more than 1,400 Community Health Centers have the ability to test and 79% are providing walk-up or drive-up testing.
Many CHCs have also been working in partnership with stakeholders such as businesses, local health departments, the National Guard and growers to test workers at major food businesses where crowded work spaces can quickly become hot zones. Community Health Center mobile testing sites have popped up in farm fields and meat and poultry processing plants, wherever workers are at risk for exposure.
As of late July 2020, Community Health Centers across the country have tested 1,970,404 patients and 277,655 have tested positive; 60% of them were racial and ethnic minorities. African Americans and Latinx Americans are bearing the brunt of this virus with higher rates of infections and hospitalizations. Many of them are essential workers in areas such as food, agriculture, service industries and other necessary frontline jobs.

One of many mobile testing sites hosted by Charter Oak Community Health Center in Hartford, Connecticut.
As spikes continue and hospitals in some states are overwhelmed, CHCs have operated as shock absorbers, caring for non-acute COVID patients and connecting them to services such as housing or food pantries as they and their families self-quarantine. Telehealth has emerged as a vital force connecting CHCs to their patients during the COVID-19 pandemic, as shelter in place restrictions nationwide have limited patients’ ability to access health care services in person.
At the height of the pandemic, 98% of CHCs across the U.S. held virtual visits. Federal health insurance payers such as Medicare and Medicaid, with the help of Congressional lawmakers, also rapidly amended billing rules to grant more flexibility and boost reimbursement rates for telemedicine. These actions, as well as targeted funding from the Federal Communications Commission, helped soften the staggering financial blows CHCs sustained during the pandemic while boosting broadband connectivity in hard-to-reach communities.
Community Health Centers have fought COVID-19 despite a host of challenges that include a chronic shortage of protective gear, medical supplies, thin operating budgets and short- term funding extensions that make planning for future pandemics nearly impossible. They will continue to nimbly pivot and launch innovations to ease the daily inequities faced by more than 30 million Americans including major challenges in accessing the U.S. health care system.
[/cs_text][/cs_element_layout_column][/cs_element_layout_row][cs_element_layout_row _id=”82″ ][cs_element_layout_column _id=”83″ ] [/cs_element_layout_column][cs_element_layout_column _id=”84″ ][cs_text]
Somerset West CHC anchors COVID 19 response in commitment to tackling anti-Black racism
[/cs_text][/cs_element_layout_column][cs_element_layout_column _id=”86″ ] [/cs_element_layout_column][/cs_element_layout_row][cs_element_layout_row _id=”87″ ][cs_element_layout_column _id=”88″ ][x_columnize]
 In 2017, the United Nations released a report on the status of anti-Black racism in Canada noting: “History informs anti-black racism and racial stereotypes that are so deeply entrenched in institutions, policies and practices, that its institutional and systemic forms are either functionally normalized or rendered invisible, especially to the dominant group.”
In 2017, the United Nations released a report on the status of anti-Black racism in Canada noting: “History informs anti-black racism and racial stereotypes that are so deeply entrenched in institutions, policies and practices, that its institutional and systemic forms are either functionally normalized or rendered invisible, especially to the dominant group.”
The legacy of anti-Black racism in Canada manifests as a lack of opportunity, poorer physical and mental health outcomes, lower socio-economic status, precarious employment, higher unemployment, higher poverty rates, and over-representation in the prison, mental healthcare, and child welfare systems.
Structural inequities that exist within Black communities across Canada have been further amplified during the COVID 19 global pandemic.
In Ottawa, preliminary data this June from Ottawa Public Health revealed that 66% of COVID-19 patients in the city are from a racialized (ethnocultural) community, while 54% are immigrants. Across the province of Ontario, reporting from Public Health Ontario has also recently shown that the impact of COVID-19 on the most ethno-culturally diverse neighbourhoods in the province is significantly greater than on less diverse neighbourhoods: infection and related deaths are three times higher; hospitalization rates are four times higher; ICU admission rates are four times higher.
In early April, a prominent group of Black health professionals and leaders from Community Health Centres across the province of Ontario — including Somerset West CHC’s Director of Primary Health Care and Regional Programs, Suzanne Obiorah — penned an open letter and statement, warning authorities about the potential for COVID-19 to disproportionately impact Black communities.
The underlying reasons for these disparities are complex and multi-factorial. What’s clear is that we need to go beyond simply highlighting the disparities. We need to actively mobilize in narrowing and ultimately eliminating them.
In Ottawa, as elsewhere, members of the diverse Black community experience systemic barriers in accessing health services, and services that are culturally competent and informed by anti-racist and anti-oppressive approaches.
Somerset West Community Health Centre has worked hard over the past 15 years to address and undo these systemic barriers, starting with its own organization and services.
Working collaboratively with diverse members and groups within the Black community, Somerset West CHC has engaged in forums and programs over the years to document experiences with the health system.
 Members of the Black community continue to share experiences of hurt, distrust, pain and raw emotions related encounters with healthcare and other social systems. For instance, how they are dismissed when seeking pain treatment for sickle cell; how Black children are frequently misdiagnosed with behavioural problems because the symptoms they display in school do not match with current assessment tools used to diagnose learning disabilities. And, how cancer screening often gets missed or occurs less frequently in Black women. And, how mental illness is often undiagnosed or misdiagnosed because of a lack of cultural understanding. The list goes on.
Members of the Black community continue to share experiences of hurt, distrust, pain and raw emotions related encounters with healthcare and other social systems. For instance, how they are dismissed when seeking pain treatment for sickle cell; how Black children are frequently misdiagnosed with behavioural problems because the symptoms they display in school do not match with current assessment tools used to diagnose learning disabilities. And, how cancer screening often gets missed or occurs less frequently in Black women. And, how mental illness is often undiagnosed or misdiagnosed because of a lack of cultural understanding. The list goes on.
Prior to COVID-19, Somerset West CHC had been playing an important role in addressing and working to remove these systemic barriers. A major focus had been mental health where, for example, the CHC has retained a Black mental health outreach worker to increase culturally-responsive mental health supports for members of the Black community.
As the COVID-19 pandemic began to set in, the CHC knew that it would need to ground its supports within its commitment to anti-Black racism. The CHC partnered with six agencies to hold a series of live Facebook events in order to share information and experiences related to COVID-19 in the Black community. The virtual series has been held bi-weekly and creates a safe space to share experiences and education on a variety of COVID-19 related topics.
The CHC also launched a support line, staffed by a Black Mental Health professional, to offer practical assistance, resource navigation, crisis support, health coaching and supportive counselling. The staff member is actively engaged with community leaders and organizations, seeking to reach out and respond to individual and family issues that surface as a direct result o f COVID-19.
f COVID-19.
The horrendous killing of George Floyd in the United States sparked a global movement which has added another layer of complexity and trauma for individuals impacted by anti-Black racism.
In solidarity with Ottawa’s Black Lives Matter movement, Somerset West CHC has partnered with Black-led organizations, Black community associations and other committed agencies to coordinate a community response to these intersecting traumas.
Together, partners first mapped out individual organizations responding to these crises and identified gaps in services and supports specifically related to the mental health and wellbeing of Black communities. They identified a need for a more holistic, collective, and regional approach and agreed to work together to align and coordinate their responses and advocate for systemic change.
Since then, partners have coordinated a number of responses including wellness checks in identified neighbourhoods, offering basic supplies for those in need, addressing food security, responding to crisis and providing mental health supports.
So much more still needs to be done but out of these intersecting crises have emerged new partnerships, and a growing commitment to support members of the Black community to claim space, and to find healing and equity grounded in their diversity, complexity and intersectionality.
Now more than ever, in Ottawa and everywhere, communities need appropriate services, informed through the lens of anti-Black racism and anti-oppression.
[/x_columnize][/cs_element_layout_column][/cs_element_layout_row][cs_element_layout_row _id=”90″ ][cs_element_layout_column _id=”91″ ][cs_text]
It takes a village: partnering to ensure food security in Kingston, Canada
 Kathy Sturmey
Kathy Sturmey
Good Food Stand Coordinator, Kingston Community Health Centres (Kingston, Ontario, Canada)
When I reflect on the last four months, the saying “it takes a village” resonates with me more than ever before. In these uncertain times, we are being asked to look after each other. By wearing masks and physically distancing, we are taking care of the other members of our “village.”
The Good Food Box COVID-19 Emergency Response Initiative in our city has been “it takes a village” in action. Thirty-seven different agencies and community health professionals, including Kingston Community Health Centres, have been reaching out to their clients, patients, members, and families, making that vital first contact with vulnerable people – letting them know we are here and we care. All partners are offering a crucial link to healthy and accessible food for community members who are or are at risk of becoming food insecure.
 Every other Thursday, a team of 35 mask-wearing, sanitizer-toting, social-distancing volunteers from our Community Health Centre and two partner groups — Loving Spoonful and Limestone District School Board — convene at Kingston CHCs to pack, sort, and distribute over 250 boxes of healthy fruits and vegetables throughout the Kingston area from east of Highway 15 to Amherstview and Odessa.
Every other Thursday, a team of 35 mask-wearing, sanitizer-toting, social-distancing volunteers from our Community Health Centre and two partner groups — Loving Spoonful and Limestone District School Board — convene at Kingston CHCs to pack, sort, and distribute over 250 boxes of healthy fruits and vegetables throughout the Kingston area from east of Highway 15 to Amherstview and Odessa.
Satellite volunteers deliver boxes to members of the Indigenous community, and neighbouring communities of Verona, Sydenham, Napanee, and Cloyne.
Online customers of the Good Food Box affordable access program purchase boxes for themselves and for their neighbours in need, saying things like:
- One box we are gifting to another person who can’t afford it… I appreciate this initiative.
- We donated the second box to the Kingston Youth Shelter. My kids decided we should. 🙂
It takes a village…
To date we have distributed 1240 Good Food Boxes to individuals and families in the region. We were able to deliver over 800 free boxes to the most vulnerable by the middle of June.
 This initiative has only been possible through the incredible generosity and quick response of our funders: Community Foundation for Kingston & Area; the Regina Rosen Food First Fund; United Way KFL&A; Meal Exchange and Community Food Centres Canada.
This initiative has only been possible through the incredible generosity and quick response of our funders: Community Foundation for Kingston & Area; the Regina Rosen Food First Fund; United Way KFL&A; Meal Exchange and Community Food Centres Canada.
Without the support of these donors, the reach and flexibility of “boots on the ground” initiatives like the Good Food Box would be greatly diminished.
The Good Food Box team is grateful to Kingston CHCs management for allowing use of large meeting rooms to work while maintaining social distancing guidelines, and to Mike Coughlin at our centre as well as greeters/screeners who welcome our volunteer drivers every Thursday!
[/cs_text][/cs_element_layout_column][cs_element_layout_column _id=”93″ ][cs_text]
Connecting families and children in Ottawa, Canada with supports during the pandemic
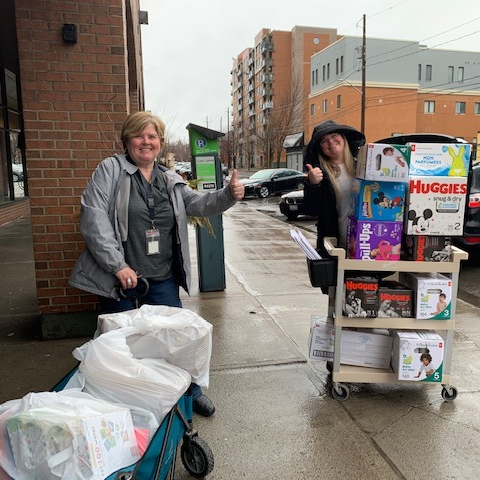 The Early Years and EarlyON team at Centretown Community Health Centre in Ottawa, Ontario, Canada is committed to providing families and children with daily support and services. During the pandemic, the team has worked collaboratively with other teams at the CHC to help families successfully navigate community resources and a wide range of challenging circumstances.
The Early Years and EarlyON team at Centretown Community Health Centre in Ottawa, Ontario, Canada is committed to providing families and children with daily support and services. During the pandemic, the team has worked collaboratively with other teams at the CHC to help families successfully navigate community resources and a wide range of challenging circumstances.
Families in the region are living through a time of uncertainty, overwhelmed, stressed and isolated all while trying to keep children physically and mentally well. The team has provided families with information about early childhood development, parenting support and education, outreach services and service navigation.
From the outset of the pandemic the Early Years and EarlyON team was actively engaged in helping develop Centretown CHC’s pandemic plan.
As the Ottawa region entered into a lockdown period beginning this March, the team diligently assessed where needs were emerging in the community and began right away to offer their support.
Emergency baby supplies were made easily accessible for families, including diapers, wipes, breastfeeding supplies and clothing. Deliveries were made for families who were faced with barriers accessing food and emergency supplies. Early Learning Activity Kits were put together by the team to support at home learning for families. The team completed wellness calls to provide virtual support and navigation for services across Ottawa.
And, as warmer weather began to arrive, Physical Activity Kits were created in order to promote outdoor physical activity for families all while practicing physical distancing measures.
 Direct services at the CHC which were deemed essential for community members with young children were adapted and continued through new methods. Breastfeeding support, as well as, pre and postnatal support were continued by telephone to support new and expecting mothers on an ongoing basis.
Direct services at the CHC which were deemed essential for community members with young children were adapted and continued through new methods. Breastfeeding support, as well as, pre and postnatal support were continued by telephone to support new and expecting mothers on an ongoing basis.
The CHC’s Welcome Baby Prenatal Nutrition Program continued providing support to participants, including delivery of a monthly healthy snack pack and a weekly phone call to each participant. And, with an increased demand for baby weight services, the team offered a weekly self-serve baby weight station at the CHC.
As the status of the pandemic continues to evolve, Centretown CHC’s Early Years and EarlyOn team continues to adjust and adapt these services, programs and supports to meet the evolving needs of local families. The team has connected with over 100 families over the past few months and continues to build relationships with community members in hopes to provide a sense of security and comfort for all. The ultimate goal for the Early Years and EarlyOn team is to foster healthy and happy children and families.
[/cs_text][/cs_element_layout_column][/cs_element_layout_row][/cs_element_section][cs_element_section _id=”95″ ][cs_element_layout_row _id=”96″ ][cs_element_layout_column _id=”97″ ][x_custom_headline level=”h2″ looks_like=”h3″ accent=”false” class=”cs-ta-center” style=”color: hsl(0, 0%, 100%);”]Current IFCHC Members[/x_custom_headline][/cs_element_layout_column][/cs_element_layout_row][/cs_element_section][cs_element_section _id=”99″ ][cs_element_layout_row _id=”100″ ][cs_element_layout_column _id=”101″ ][cs_text]
Click here for information on becoming a member
Happy National Community Health Centers Week to our U.S. Members!
Battling the COVID-19 Pandemic on the Frontlines in South Los Angeles, USA
Located in south Los Angeles (South LA), California, USA, St. John’s Well Child & Family Center is a network of 19 federally-qualified Community Health Centres providing care and support to a wide range of community members within the largest area of poverty in the United States.
This multi-faceted Community Health Centre has been steadfastly committed to responding to the desperate need for COVID-19 services locally. Decades of racial and social inequality have resulted in a disproportionately high incidence of COVID-19 among South LA’s predominantly Latinx and African-American population. In fact, 47% of COVID-19 deaths come from the Latinx community in Los Angeles County while African-Americans represent 11% of all COVID-19 deaths but only 8% of the population.
To reduce the pandemic’s impact, St. John’s responded swiftly and decisively in early March when the first cases of community transmission were reported. South Los Angeles is home to more than 1.5 million people and has the highest poverty rates in the United States.
“To successfully control COVID-19, we mobilized early to keep all of our communities safe and healthy,” affirms Jim Mangia, President and Chief Executive Officer of St. John’s. “We needed to marshal our resources to help the most vulnerable first to reduce infection rates and keep our community safe.”
St. John’s started by addressing the safety of its 600 staff and over 85,000 patients at 17 fixed sites and two mobile clinics. An internal COVID-19 Preparation Task Force was convened, comprised of key staff from every department, who led the complete retooling of the organization and redesigned every system and workflow in response to the pandemic.
St. John’s purchased Personal Protective Equipment (PPE) from national and international sources and received in-kind donations as well, enabling the agency to secure a six-month stockpile of PPE and sanitation supplies. Facilities staff erected isolation tents outside each fixed site to conduct testing and triage. Patients were screened and provided with face masks and screened before entering the clinics.
St. John’s initially had extremely limited access to COVID-19 testing kits at the beginning of the pandemic, especially in comparison with more affluent areas of the city. With support from local and state government agencies, augmented by St. John’s persistence in finding a new partner for test kits, the organization was able to secure enough kits to offer COVID-19 tests to everyone.
St. John’s started testing in late March. By early April, they were testing 600 residents of south Los Angeles each day. To date, St. John’s has tested 30,000 people for COVID-19 with a positivity rate of 16.63%. St. John’s is now one the largest providers of COVID testing and services of any Community Health Centre in the county.
Patients who test positive are scheduled for follow-up medical appointments (either telehealth or face-to-face depending on patient needs). In addition, St. John’s established a telehealth Command Center, comprised of five teams of receptionists, medical assistants, and providers. Command Center staff respond to all COVID-related calls from patients and community members, answering questions, assessing any symptoms, and scheduling them as needed for testing and/or a full consultation.
A Contact Tracing initiative was implemented to support the massive testing campaign that St. John’s is conducting. Contact Tracers call every COVID-positive patient to interview them regarding the people with whom they have been in contact. They then call each of those contacts to inform them of their exposure, provide them with education, answer their questions and assess them for symptoms. The initiative started in May to slow down the virus spread and identify potential viral clusters. To date, the initiative has contacted 25,366 individuals and scheduled 16,760 of the contacts for COVID-19 tests.
St. John’s started offering telehealth medicine to patients in late March to allow for continued service provision, initially conducted through telephony, Zoom, WhatsApp and FaceTime. A grant from the U.S. Federal Communications Commission allowed for the implementation of telehealth services that interface with St. John’s Electronic Health Record system as well as provide remote monitoring of patients with positive COVID tests and symptoms. Telehealth allows continued access to quality care for a community with limited available resources while helping reduce COVID-19 infection rates.
“The financial cost to St. John’s for responding to this pandemic is high,” says Mr. Mangia. “But the cost of not responding will be unfathomable and devastating to our community and its future. With the support of our partners, we will continue to respond as long as needed to keep South LA safe.”
Community Health Mobilizes in Melbourne, Australia
Star Health is a registered Community Health Centre located within the inner urban southeast of metropolitan Melbourne, Australia. In June 2020, the Victoria State Department of Health and Human Services (DHHS) asked Star Heath to run a COVID-19 community engagement and health promotion program in public housing across local municipalities, targeting public housing and other vulnerable communities.
“It became clear that outreach testing along with community engagement and support was going to be required,” says Sarah Fair, Star Health’s General Manager for Healthy Communities. “We needed to integrate several components into a robust program”.
As a result, Star Health created a Mobile COVID Testing Team (MCTT). Within the first 3 weeks of operations the team implemented 5 pop-up clinics per week. The organisation was then asked by the Regional Director of DHHS to ‘supercharge’ operations. This saw the creation of 13 clinics, spread across various locations, including extending operations in larger public housing high-rise buildings.
The focus of its program has been modified to cover other vulnerable communities including community housing projects, indigenous people, injecting drug users, sex workers and novel locations (for example near homelessness food services). A Testing Bus has been created to accommodate the requirements of a roving testing team.
The MCTT also provides free transport for community members to fixed testing clinics 7 days a week in partnership with St Johns Ambulance. In addition, Star Health provides a Stay Connected line which offers psychosocial support, primary care and care coordination to any vulnerable community member during the pandemic.
Star Health, in partnership with DHHS Office of Housing, has also established a Health Concierge Service at entry/exit points at three of the largest public housing communities. This service provides: community engagement, education, screening, masks and voluntary temperature checks and referrals.
Between June 25 and July 23, the Star Health Mobile COVID Testing Team had conducted 1286 tests across public housing communities using a nurse-led model. This has seen over 50% testing coverage at some sites with over 1600 community engagements. The impacts of this work include reassuring epidemiological data on low case numbers, prevention education and linkage to care and support for many residents at risk across domains such as chronic condition care, mental health and food security.
In addition to mobile testing, as of July 23, Star Health’s fixed site COVID-19 Screening Clinic has tested over 10,000 members of the local community. “Community Health Services like ours, throughout Victoria, are very well positioned to help within these challenging times,” says Star Health’s Acting CEO, Kent Burgess.
“Our organizations have deep, local relationships, with the capacity to effectively engage with diverse segments of the community.”
As a result of these long-standing relationships in their communities, Community Health Centres like Star Health tend to have have high levels of trust and better engagement with the community, including educational programs.
Star Health has collaborated closely with social landlords (public housing managers) and used the expertise of Star Health’s Public Housing Community Capacity Building team to develop a door-to-door testing model that outreaches from the pop-up clinics. Star Health has engaged with interpreters to help support vulnerable communities who may otherwise miss out on testing. It has also produced health educational/testing promotion videos in multiple community languages to support vulnerable people who are culturally and linguistically diverse.
Community Health Centres, throughout Victoria State and more broadly in Australia, are proving their critical value to the public health system during a time when the health system is being severely tested. No one can connect communities to health care and support like community health can.
Community Health Leads Expanded COVID-19 Efforts in Soweto/Johannesburg, South Africa
When South Africa’s National Party took power in 1948 and introduced apartheid they also eliminated an impressive network of more than 40 Community Health Centres that had been established through the leadership of Drs Sidney and Emily Kark. The most famous of these was the first Community Health Centre, established by the Karks in the rural Kwa-Zulu Natal province town of Pholela.
Decades later, the post-apartheid government of South Africa implemented District Health Services with so-called “CHCs” as a key component. However, these CHCs lack many critical functions of “community-oriented primary health care (COPHC)” that are common to the CHC model around world.
That’s why, in 2013, Chiawelo Community Practice (CCP) was established within the Chiawelo CHC in Soweto, Johannesburg as an effort to begin re-building the true CHC model including COPHC. In concert with the Chiawelo CHC, Chiawelo Community Practice serves a community of ±22,000 people and is staffed by a part-time family physician, a clinical associate, two intern doctors rotating weekly, and more than 20 Community Health Workers (CHWs) who work under the guidance of a junior nurse team leader.
The Chiawelo Community Practice team delivers people-centred care to ±1,000 patients per month, with CHWs playing a critical role in health promotion, community engagement, and continuity of care. This has included setting up five health clubs in the community with ±150 elderly chronic patients involved in daily exercise, diet, and social sessions to combat social isolation.
With the onset on COVID-19, CHWs have been relied on heavily to support clients and the community. As part of their daily outreach activities, linking community members with services at the Chiawelo Community Practice clinic, CHWs have integrated COVID-19 screening. Each CHW aims for a daily goal of 14 client screenings, in addition to their other daily activities. CHWs have also been critical in staffing COVID-19 screening stations at the entrance of Chiawelo CHC and other clinics throughout Soweto.
Given the elevated risks from COVID-19 to patients with chronic and immuno-compromised conditions, Johannesburg region health authorities have tapped the team at Chiawelo Community Practice to expand home-based care and delivery of medications.
“We have a lot of experience to draw from already,” says Dr, Shabir Moosa, lead physician responsible for creation of Chiawelo Community Practice. “We have taken lessons and practices developed here and have developed a home-based Case Management Plan for chronic care patients throughout Johannesburg.”
Led by nursing team leaders, with delivery of medicines by CHWs, the plan is slated for roll out this August, with scale-up across Johannesburg over the months ahead.
Victoria, Canada’s Cool Aid Turns on a Dime
Some members of Cool Aid’s medical and health team stand together, while apart, in Victoria, Canada during COVID-19.
When your Community Health Centre has 20 locations, a staff compliment of 350, and 12,000 clients to support who are marginalized, many experiencing homelessness, it’s hard to turn on a dime. But that’s exactly what Victoria Cool Aid Society (Victoria, British Columbia, Canada) did when public health authorities ordered a shut down of businesses and many services throughout the province of British Columbia during the onset of the COVID-19 pandemic.
Day by day, the organization’s Health & Safety Manager and medical staff created new procedures to protect staff and clients from COVID-19. Staff focused on information technology made it possible for team members to quickly transition to working from home, leaning heavily on video conferencing. Human resources team members helped dozens of staff work through challenges and fears.
Cool Aid provided telemedicine options for patients, working with the provincial government to rapidly expand their Health Outreach Team to care for and support homeless and street-involved clients, both at usual encampments and new indoor spaces created as a result of the pandemic. As a Community Health Centre with tremendous focus on shelter and housing, Cool Aid also took on a new project to house 30 homeless individuals who had been camping in the city, receiving approval to build an additional 102 affordable apartment units. Housing is health care.
Several branches of the CHC went virtual, including their Downtown Community Centre and Support Services. Staff reported that relationships with clients actually deepened in many instances as clients sought and received assurances and safety information.
Riley Vaskic, an Outreach Worker at Cool Aid, notes that while COVID-19 has, unfortunately, reduced some services for clients due to physical distancing and precautions she has also seen many positive developments.
Riley Vaskic
“The pandemic has shed a lot of light for the general public on homelessness and fewer people are turning a blind eye on our clients,” Vaskic says. “They are starting to realize that the health of the most marginalized affects the health of everyone. People better understand the critical role that housing plays in health and community wellbeing.”
She also says she’s pleased that jobs that have not traditionally been recognized as frontline are now being valued more profoundly. Important jobs like the ones played by her team at Cool Aid’s REES Support Services. Team members at REES take a co-operative, recovery-based approach to help reduce people’s isolation, providing people a resource centre with accessible computers & phone, employment preparation and labour pool jobs, and assistance and advocacy navigating income assistance, disability claims, identification, and more.
“We have learned new ways of connecting with people at Cool Aid and the pandemic has illuminated what really matters in my life.”
Video and blog series from Canadian Association of Community Health Centres addresses inequitable health and social impacts of pandemic
Homelessness
Domestic Violence
Isolated Seniors
Food Insecurity
BLOG: Community Health Centres take swift action to protect Canada’s homeless during the pandemic
BLOG: Community Health Centres address surge in domestic violence, call for attention to systemic impacts of COVID-19
BLOG: Community Health Centres provide critical lifeline for isolated seniors during the pandemic
BLOG: Community Health Centres tackle surge in food insecurity across Canada during pandemic
Bromley by Bow Centre mobilizes social prescribing crisis response in London, UK
The Bromley by Bow Centre was one of the earliest pioneers of social prescribing principles and the London, UK based Community Health Centre aims to apply them in everything they do. This includes managing crisis situations.
For the CHC’s skilled social prescribing Link Workers this means taking time to get to know a person, giving them space to make sense of their situation and feelings, then jointly developing a plan to help the person access the right information and support.
Social prescribing was developed in recognition that the majority of factors affecting mental and physical ill health are social and economic. People need friends and a feeling of belonging, a sense of purpose, financial security, a safe home and hope for their future. The term refers to a process whereby healthcare professionals refer patients to a range of local, non-clinical services in order to improve their health and wellbeing.
Bromley by Bow’s social prescribing service is usually triggered by a referral from a health professional. However, during the COVID-19 crisis, a combined Health Partnership and Social Prescribing team at the centre began a project to actively reach out to patients. People were identified, using health data and local knowledge, as having additional risk of social and economic vulnerability due to lock down measures.
People were contacted by the social prescribing health team by phone. These phone calls were widely welcomed and uncovered a higher level of distress and need than was expected with many respondents living on their own and feeling isolated and scared. Many people required help for essential needs such as food deliveries and help with accessing health advice. They also needed reassurance during an anxious time and a sense they were not alone. The organization developed a “Home Pack” to support local community members with online resources.
Food bank set up at Bromley by Bow Centre, one of many important services scaled through social prescribing crisis response.
During a ten-week period from late March to early June, 704 calls were made and 512 people in the age range of 9- 90 years were spoken with by team members. These were people who may not otherwise have been contacted during lock down and many were suffering in silence.
Once the social prescribing health team engaged with people, they were able to activate emergency food supplies from the Food Bank and other services from the organization and partner agencies.
Many local residents report that it was the conversation itself, the human connection, that they valued most valued during a troubling time. An interim report from the centre details a wide range of observations, outcomes, and lessons learned from the COVID-19 social prescribing crisis response.
America’s CHCs lead national testing and care efforts for vulnerable communities
Since COVID-19 struck, Community Health Centers in rural and urban areas across the U.S. have pivoted to address the pandemic, launching drive-through and curbside testing sites and delivering 160,000 COVID tests per week. According to the latest research and findings from the U.S. National Association of Community Health Centers, 94% of America’s more than 1,400 Community Health Centers have the ability to test and 79% are providing walk-up or drive-up testing.
Many CHCs have also been working in partnership with stakeholders such as businesses, local health departments, the National Guard and growers to test workers at major food businesses where crowded work spaces can quickly become hot zones. Community Health Center mobile testing sites have popped up in farm fields and meat and poultry processing plants, wherever workers are at risk for exposure.
As of late July 2020, Community Health Centers across the country have tested 1,970,404 patients and 277,655 have tested positive; 60% of them were racial and ethnic minorities. African Americans and Latinx Americans are bearing the brunt of this virus with higher rates of infections and hospitalizations. Many of them are essential workers in areas such as food, agriculture, service industries and other necessary frontline jobs.
One of many mobile testing sites hosted by Charter Oak Community Health Center in Hartford, Connecticut.
As spikes continue and hospitals in some states are overwhelmed, CHCs have operated as shock absorbers, caring for non-acute COVID patients and connecting them to services such as housing or food pantries as they and their families self-quarantine. Telehealth has emerged as a vital force connecting CHCs to their patients during the COVID-19 pandemic, as shelter in place restrictions nationwide have limited patients’ ability to access health care services in person.
At the height of the pandemic, 98% of CHCs across the U.S. held virtual visits. Federal health insurance payers such as Medicare and Medicaid, with the help of Congressional lawmakers, also rapidly amended billing rules to grant more flexibility and boost reimbursement rates for telemedicine. These actions, as well as targeted funding from the Federal Communications Commission, helped soften the staggering financial blows CHCs sustained during the pandemic while boosting broadband connectivity in hard-to-reach communities.
Community Health Centers have fought COVID-19 despite a host of challenges that include a chronic shortage of protective gear, medical supplies, thin operating budgets and short- term funding extensions that make planning for future pandemics nearly impossible. They will continue to nimbly pivot and launch innovations to ease the daily inequities faced by more than 30 million Americans including major challenges in accessing the U.S. health care system.
Somerset West CHC anchors COVID 19 response in commitment to tackling anti-Black racism
In 2017, the United Nations released a report on the status of anti-Black racism in Canada noting: “History informs anti-black racism and racial stereotypes that are so deeply entrenched in institutions, policies and practices, that its institutional and systemic forms are either functionally normalized or rendered invisible, especially to the dominant group.”
The legacy of anti-Black racism in Canada manifests as a lack of opportunity, poorer physical and mental health outcomes, lower socio-economic status, precarious employment, higher unemployment, higher poverty rates, and over-representation in the prison, mental healthcare, and child welfare systems.
Structural inequities that exist within Black communities across Canada have been further amplified during the COVID 19 global pandemic.
In Ottawa, preliminary data this June from Ottawa Public Health revealed that 66% of COVID-19 patients in the city are from a racialized (ethnocultural) community, while 54% are immigrants. Across the province of Ontario, reporting from Public Health Ontario has also recently shown that the impact of COVID-19 on the most ethno-culturally diverse neighbourhoods in the province is significantly greater than on less diverse neighbourhoods: infection and related deaths are three times higher; hospitalization rates are four times higher; ICU admission rates are four times higher.
Suzanne Obiorah, director of primary health care and regional programs at the Somerset West CHC
In early April, a prominent group of Black health professionals and leaders from Community Health Centres across the province of Ontario — including Somerset West CHC’s Director of Primary Health Care and Regional Programs, Suzanne Obiorah — penned an open letter and statement, warning authorities about the potential for COVID-19 to disproportionately impact Black communities.
The underlying reasons for these disparities are complex and multi-factorial. What’s clear is that we need to go beyond simply highlighting the disparities. We need to actively mobilize in narrowing and ultimately eliminating them.
In Ottawa, as elsewhere, members of the diverse Black community experience systemic barriers in accessing health services, and services that are culturally competent and informed by anti-racist and anti-oppressive approaches.
Somerset West Community Health Centre has worked hard over the past 15 years to address and undo these systemic barriers, starting with its own organization and services.
Working collaboratively with diverse members and groups within the Black community, Somerset West CHC has engaged in forums and programs over the years to document experiences with the health system.
Members of the Black community continue to share experiences of hurt, distrust, pain and raw emotions related encounters with healthcare and other social systems. For instance, how they are dismissed when seeking pain treatment for sickle cell; how Black children are frequently misdiagnosed with behavioural problems because the symptoms they display in school do not match with current assessment tools used to diagnose learning disabilities. And, how cancer screening often gets missed or occurs less frequently in Black women. And, how mental illness is often undiagnosed or misdiagnosed because of a lack of cultural understanding. The list goes on.
Prior to COVID-19, Somerset West CHC had been playing an important role in addressing and working to remove these systemic barriers. A major focus had been mental health where, for example, the CHC has retained a Black mental health outreach worker to increase culturally-responsive mental health supports for members of the Black community.
As the COVID-19 pandemic began to set in, the CHC knew that it would need to ground its supports within its commitment to anti-Black racism. The CHC partnered with six agencies to hold a series of live Facebook events in order to share information and experiences related to COVID-19 in the Black community. The virtual series has been held bi-weekly and creates a safe space to share experiences and education on a variety of COVID-19 related topics.
The CHC also launched a support line, staffed by a Black Mental Health professional, to offer practical assistance, resource navigation, crisis support, health coaching and supportive counselling. The staff member is actively engaged with community leaders and organizations, seeking to reach out and respond to individual and family issues that surface as a direct result of COVID-19.
The horrendous killing of George Floyd in the United States sparked a global movement which has added another layer of complexity and trauma for individuals impacted by anti-Black racism.
In solidarity with Ottawa’s Black Lives Matter movement, Somerset West CHC has partnered with Black-led organizations, Black community associations and other committed agencies to coordinate a community response to these intersecting traumas.
Together, partners first mapped out individual organizations responding to these crises and identified gaps in services and supports specifically related to the mental health and wellbeing of Black communities. They identified a need for a more holistic, collective, and regional approach and agreed to work together to align and coordinate their responses and advocate for systemic change.
Since then, partners have coordinated a number of responses including wellness checks in identified neighbourhoods, offering basic supplies for those in need, addressing food security, responding to crisis and providing mental health supports.
So much more still needs to be done but out of these intersecting crises have emerged new partnerships, and a growing commitment to support members of the Black community to claim space, and to find healing and equity grounded in their diversity, complexity and intersectionality.
Now more than ever, in Ottawa and everywhere, communities need appropriate services, informed through the lens of anti-Black racism and anti-oppression.
It takes a village: partnering to ensure food security in Kingston, Canada
Kathy Sturmey
Good Food Stand Coordinator, Kingston Community Health Centres (Kingston, Ontario, Canada)
When I reflect on the last four months, the saying “it takes a village” resonates with me more than ever before. In these uncertain times, we are being asked to look after each other. By wearing masks and physically distancing, we are taking care of the other members of our “village.”
The Good Food Box COVID-19 Emergency Response Initiative in our city has been “it takes a village” in action. Thirty-seven different agencies and community health professionals, including Kingston Community Health Centres, have been reaching out to their clients, patients, members, and families, making that vital first contact with vulnerable people – letting them know we are here and we care. All partners are offering a crucial link to healthy and accessible food for community members who are or are at risk of becoming food insecure.
Every other Thursday, a team of 35 mask-wearing, sanitizer-toting, social-distancing volunteers from our Community Health Centre and two partner groups — Loving Spoonful and Limestone District School Board — convene at Kingston CHCs to pack, sort, and distribute over 250 boxes of healthy fruits and vegetables throughout the Kingston area from east of Highway 15 to Amherstview and Odessa.
Satellite volunteers deliver boxes to members of the Indigenous community, and neighbouring communities of Verona, Sydenham, Napanee, and Cloyne.
Online customers of the Good Food Box affordable access program purchase boxes for themselves and for their neighbours in need, saying things like:
One box we are gifting to another person who can’t afford it… I appreciate this initiative.
We donated the second box to the Kingston Youth Shelter. My kids decided we should. 🙂
It takes a village…
To date we have distributed 1240 Good Food Boxes to individuals and families in the region. We were able to deliver over 800 free boxes to the most vulnerable by the middle of June.
This initiative has only been possible through the incredible generosity and quick response of our funders: Community Foundation for Kingston & Area; the Regina Rosen Food First Fund; United Way KFL&A; Meal Exchange and Community Food Centres Canada.
Without the support of these donors, the reach and flexibility of “boots on the ground” initiatives like the Good Food Box would be greatly diminished.
The Good Food Box team is grateful to Kingston CHCs management for allowing use of large meeting rooms to work while maintaining social distancing guidelines, and to Mike Coughlin at our centre as well as greeters/screeners who welcome our volunteer drivers every Thursday!
Connecting families and children in Ottawa, Canada with supports during the pandemic
The Early Years and EarlyON team at Centretown Community Health Centre in Ottawa, Ontario, Canada is committed to providing families and children with daily support and services. During the pandemic, the team has worked collaboratively with other teams at the CHC to help families successfully navigate community resources and a wide range of challenging circumstances.
Families in the region are living through a time of uncertainty, overwhelmed, stressed and isolated all while trying to keep children physically and mentally well. The team has provided families with information about early childhood development, parenting support and education, outreach services and service navigation.
From the outset of the pandemic the Early Years and EarlyON team was actively engaged in helping develop Centretown CHC’s pandemic plan.
As the Ottawa region entered into a lockdown period beginning this March, the team diligently assessed where needs were emerging in the community and began right away to offer their support.
Emergency baby supplies were made easily accessible for families, including diapers, wipes, breastfeeding supplies and clothing. Deliveries were made for families who were faced with barriers accessing food and emergency supplies. Early Learning Activity Kits were put together by the team to support at home learning for families. The team completed wellness calls to provide virtual support and navigation for services across Ottawa.
And, as warmer weather began to arrive, Physical Activity Kits were created in order to promote outdoor physical activity for families all while practicing physical distancing measures.
Direct services at the CHC which were deemed essential for community members with young children were adapted and continued through new methods. Breastfeeding support, as well as, pre and postnatal support were continued by telephone to support new and expecting mothers on an ongoing basis.
The CHC’s Welcome Baby Prenatal Nutrition Program continued providing support to participants, including delivery of a monthly healthy snack pack and a weekly phone call to each participant. And, with an increased demand for baby weight services, the team offered a weekly self-serve baby weight station at the CHC.
As the status of the pandemic continues to evolve, Centretown CHC’s Early Years and EarlyOn team continues to adjust and adapt these services, programs and supports to meet the evolving needs of local families. The team has connected with over 100 families over the past few months and continues to build relationships with community members in hopes to provide a sense of security and comfort for all. The ultimate goal for the Early Years and EarlyOn team is to foster healthy and happy children and families.
Current IFCHC Members
Organization Type of Member Town (HQ) State/Prov Country Website Twitter
Community Health AustraliaNational CHC AssociationMelbourneVictoriaAustraliacommunityhealth.org.auTwitter Profile
Victorian Healthcare AssociationRegional/State/Provincial CHC AssociationMelbourbeVictoriaAustraliavha.org.auTwitter Profile
Star HealthCommunity Health CentreMelbourneVictoriaAustraliastarhealth.org.auTwitter Profile
Merri HealthCommunity Health CentreCoburgVictoriaAustraliamerrihealth.org.auTwitter Profile
cohealthCommunity Health CentreCollingwoodVictoriaAustraliacohealth.org.auTwitter Profile
North Richmond Community HealthCommunity Health CentreRichmondVictoriaAustralianrch.com.auTwitter Profile
IPC HealthCommunity Health CentreDeer ParkVictoriaAustraliaipchealth.com.auTwitter Profile
Flemish Association of Neighborhood Health CentersRegional/State/Provincial CHC AssociationBrusselsCapital RegionBelgiumvwgc.be
The Alex Community Health CentreCommunity Health CentreCalgaryAlbertaCanadathealex.caTwitter Profile
British Columbia Association of Community Health CentresRegional/State/Provincial CHC AssociationVictoriaBritish ColumbiaCanadabcachc.orgTwitter Profile
Victoria Cool Aid SocietyCommunity Health CentreVictoriaBritish ColumbiaCanadacoolaid.orgTwitter Profile
Manitoba Association of Community HealthRegional/State/Provincial CHC AssociationWinnipegManitobaCanadamachmb.caTwitter Profile
Canadian Association of Community Health CentresNational CHC AssociationTorontoOntarioCanadacachc.caTwitter Profile
Centretown Community Health CentreCommunity Health CentreOttawaOntarioCanadacentretownchc.orgTwitter Profile
Somerset West Community Health CentreCommunity Health CentreOttawaOntarioCanadaswchc.on.caTwitter Profile
TAIBU Community Health CentreCommunity Health CentreScarboroughOntarioCanadataibuchc.caTwitter Profile
Centre de santé communautaire du TémiskamingCommunity Health CentreNew LiskeardOntarioCanadacsctim.on.caTwitter Profile
Access Alliance Multicultural Health and Community ServicesCommunity Health CentreTorontoOntarioCanadaaccessalliance.caTwitter Profile
Langs Community Health WellnessCommunity Health CentreCambridgeOntarioCanadalangs.orgTwitter Profile
Wellfort Community Health ServicesCommunity Health CentreBramptonOntarioCanadawellfort.caTwitter Profile
South Riverdale Community Health CentreCommunity Health CentreTorontoOntarioCanadasrchc.caTwitter Profile
South-East Ottawa Community Health CentreCommunity Health CentreOttawaOntarioCanadaseochc.on.caTwitter Profile
Kingston Community Health CentresCommunity Health CentreKingtonOntarioCanadakchc.caTwitter Profile
Belleville and Quinte West Community Health CentreCommunity Health CentreBellevilleOntarioCanadabqwchc.comTwitter Profile
NorWest Community Health CentresCommunity Health CentreThunder BayOntarioCanadanorwestchc.org
Stonegate Community Health CentreCommunity Health CentreTorontoOntarioCanadastonegatechc.orgTwitter Profile
Southwest Ontario Aboriginal Health Access CentreCommunity Health CentreLondonOntarioCanadasoahac.on.ca
Seaway Valley Community Health CentreCommunity Health CentreCornwallOntarioCanadaseawayvalleychc.caTwitter Profile
Kosrae Community Health CenterCommunity Health CentreKosraeFederated StatesMicronesiakosraechc.orgTwitter Profile
Migrant Health Center, Western RegionCommunity Health CentreMayaguezPuerto RicoPuerto Ricomigrantspr.com
Centre de santé communautaire de FadiaCommunity Health CentreDakarRégion de DakarSenegalacdev-inter.org
Centre de santé communaitaire de FatickCommunity Health CentreKaolackRégion de KaolackSenegalacdev-inter.org
Centre de santé communautaire Eva Marie Coll SeckCommunity Health CentreYeumbeulRégion de LougaSenegalacdev-inter.org
Chiawelo Community PracticeCommunity Health CentreJohannesburgGautengSouth Africaafrophc.org
Bromley by Bow CentreCommunity Health CentreLondonEnglandUnited Kingdombbbc.org.ukTwitter Profile
St. John’s Well Child and Family CenterCommunity Health CentreLos AngelesCaliforniaUnited Stateswellchild.orgTwitter Profile
Community Health Association of Mountain/Plains StatesRegional/State/Provincial CHC AssociationDenverColoradoUnited Stateschampsonline.org
Mountain Family Health CentersCommunity Health CentreGlenwood SpringsColoradoUnited Statesmountainfamily.orgTwitter Profile
Community Health Center Inc.Community Health CentreMiddletownConnecticutUnited Stateschc1.comTwitter Profile
Charter Oak Health CenterCommunity Health CentreHartfordConnecticutUnited Statesthecharteroak.orgTwitter Profile
National Association of Community Health CentresNational CHC AssociationBethesdaMarylandUnited Statesnachc.orgTwitter Profile
NEW HealthCommunity Health CentreBostonMassachusettsUnited Statesnewhealthcenter.orgTwitter Profile
Whittier Street Health CenterCommunity Health CentreRoxburyMassachusettsUnited Stateswshc.orgTwitter Profile
Greene County HealthcareCommunity Health CentreSnow HillNorth CarolinaUnited Statesgreenecountyhealthcare.comTwitter Profile
Northwest Regional Primary Care AssociationRegional/State/Provincial CHC AssociationSeattleWashingtonUnited Statesnwrpca.orgTwitter Profile
Yakima Neighborhood Health ServicesCommunity Health CentreYakimaWashingtonUnited Statesynhs.orgTwitter Profile
NorthLakes Community ClinicCommunity Health CentreIron RiverWisconsinUnited Statesnorthlakesclinic.orgTwitter Profile
Wisconsin Primary Health Care AssociationRegional/State/Provincial CHC AssociationMadisonWisconsinUnited Stateswphca.orgTwitter Profile
Organization Type of Member Town (HQ) State/Prov Country Website Twitter


















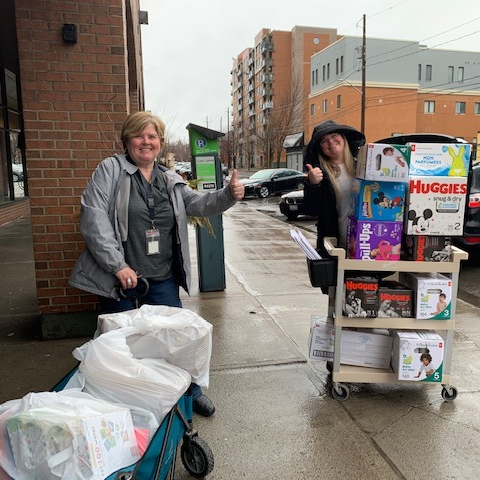
 [/cs_content_seo]
[/cs_content_seo]